Diamniotic Dichorionic and Diamniotic Monochorionic Twins: Information
Page Links: Potential Complications: Multiple Gestations, Prevalence, Factors Affecting Outcome, Placentation, References
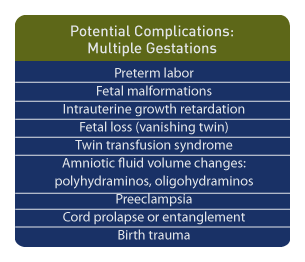
Potential Complications: Multiple Gestations
Above. Multiple gestations are at increased risk for a number of potential complications.
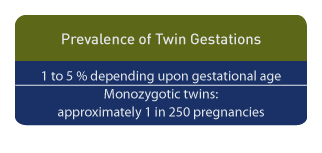
Prevalence
Depending on the gestational age at assessment, the prevalence of twin gestation varies from 1% to 5%, as a significant number of twins suffer intrauterine fetal demise of one of the pair. [1]
Monozygotic twins (derived from a single egg) occur at a relatively fixed rate of 1 in 250 pregnancies.
Factors Affecting Outcome
Above. Multiple gestations contribute to premature births and low birth weight infants. (Chart data from [2]).
The infant mortality and perinatal mortality rate among multiple births is higher than among singleton births. [3],[4] Perinatal losses are the result of early gestational age at birth, [5] and disproportionately contribute to neonatal deaths. [6]
The overall incidence of spontaneous twin gestations has declined, but assisted reproductive technologies (ART), including ovulation induction and surgical transfer of gametes or ova, have resulted in an increased number of multiple gestation pregnancies. However, recent changes in reproductive strategies have seen a moderation in the number of such pregnancies. Despite this occurrence, pregnancies after ART, including singleton ART pregnancies, are at increased risk compared to other pregnancies and require special surveillance. [7]
Placentation
Twin Placentation
Twins are derived from either a single ovum (monozygotic) or 2 ova (dizygotic). Maternal central gonadotropin levels [8],[9] influence the number of dizygotic twin pregnancies. Twin monozygotic pregnancies occur at a relatively fixed rate of approximately 1 per 250 births, and more complications occur in this group with monochorionic (MC) placentas due to placental vascular anastomosis and placental asymmetry. [10],[11]
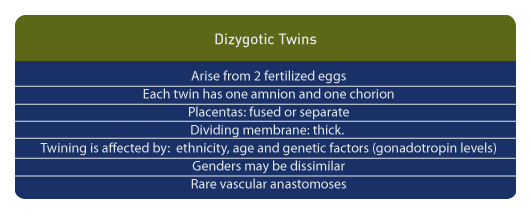
Dizygotic Twin Pregnancy
Above. Diamaniotic dichorionic twin placenta. The dividing membrane consists of 4 layers: amnion-chorion-chorion-amnion and will appear “thick” on ultrasound; the placentas can be either separate or fused.
This type of diamniotic dichorionic pregnancy arises from 2 fertilized eggs, and each twin has 1 amnion and 1 chorion; the placentas may be fused or separate and the dividing membrane is thick. This type of twinning is affected by ethnicity, age, and genetic factors such as gonadotropin levels. The genders may be dissimilar. Because dizygotic twin pregnancies arise from two entirely separate placental disks, there are rare vascular anastomoses. [10] These pregnancies account for about 80% of all twin gestations. [12] This type of placenta may also include monozygotic twins if the zygote divides early (day 2 to 3) after fertilization.
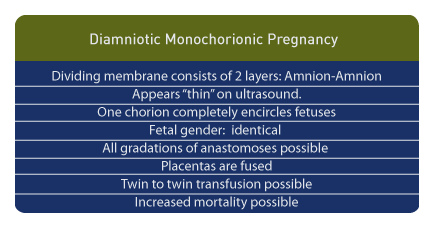
Monozygotic Twin Pregnancy
Above. Diamniotic monochorionic twin placenta. The dividing membrane consists of 2 layers: amnion-amnion, and will appear “thin” on ultrasound. There is only 1 chorion, which completely encircles the fetuses. The fetal gender is the same.
The type of placenta and the type of multiple pregnancies depend on when a single fertilized egg divides (monozygotic).
If division of the ovum occurs 2 to 3 days after fertilization, a diamniotic dichorionic (DC) gestation will result. [13]
If the division occurs between 3 to 8 days after fertilization, a diamniotic monochorionic (MC) gestation will result. [13]
If the division occurs 8 to 13 days after fertilization, a monoamniotic monochorionic gestation occurs. [13]
If the division occurs later than 13 days after fertilization, conjoined twins occur. [13]
All gradations of anastomoses are possible through the fused placentas of these pregnancies. Most cases of twin transfusion occur with diamniotic monochorionic placentation. Perinatal mortality (25-50%) occurs principally with this type of placentation, compared to the 10% mortality in the diamniotic dichorionic group. [1],[14] Recent data suggest early loss for MC exceeds the loss for dichorionic pregnancies, but after 24 weeks gestation, the differential outcomes are not different between the two groups. [15]
Monoamniotic Monochorionic Placenta
Above. In monoamniotic monochorionic twin placenta, there is no dividing membrane and the umbilical cords are entwined. The fetal gender is the same. The umbilical cords typically insert near each other and restricted fetal growth is rare.
These account for 1% of all twin pregnancies. [12] Previously mortality was reported as high as 50%, [16] but mortality can be reduced with early identification of such pregnancies.
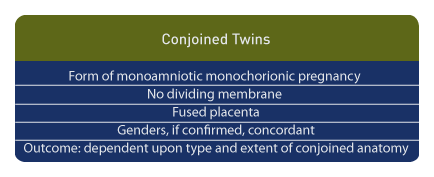
Conjoined Twins
Above. Conjoined twins are a form of monoamniotic monochorionic pregnancy with no dividing membrane and with a fused placenta. Genders, if confirmed, are concordant. Outcome depends upon which anatomic structures are conjoined.
In summary, monochorionic pregnancies result in greater fetal morbidity compared to diamniotic dichorionic pregnancies due to vascular anastomosis and placental asymmetry, at least until 24 weeks of gestation. [15]
The type of placenta as determined by ultrasound determines the frequency and severity of many multiple gestation complications. The chorion status or “chorionicity” is important to establish early in pregnancy.
About 20% of twins have monochorionic placentas. Those with diamniotic monochorionic placentas have risks that include twin transfusion syndrome and fetal growth restriction.
Other pregnancies with MC placentas are associated with higher loss rates. These include monoamniotic monochorionic (MC) placentas in which there is no dividing membrane separating the twins.
MC pregnancies also include: those discordant for congenital anomalies, conjoined twins, and twin reversed arterial perfusion (TRAP).
Determining Amnionicity and Chorionicity
In summary, the types of placental possibilities are as follows: [17]
Overall Recommendations:
The following is a summation of recommendations for multiple gestations supported by a literature review and best practices. [18]
1. Singleton growth curves are appropriate for evaluating growth.
2. Growth discordance is defined as either a 20 mm difference for abdominal circumference or 20% difference for estimated fetal weight (EFW).
3. Serial ultrasounds are appropriate for assessment of monochorionic pregnancies beginning at 16 weeks, with intervals of every 2 to 3 weeks.
4. Complications which should be referred to a tertiary care center include:
a. Twin-to-twin transfusion syndrome (TTTS).
b. Monoamniotic twin gestation.
c. Conjoined twins.
d. Twin reversed arterial perfusion (TRAP).
e. Fetal death in the second or third trimester.
f. Growth discordance in monochorionic twins.
References
-
Abstract: PMID: 2178838 -
Abstract: PMID: 15024280 -
Abstract: PMID: 12517657 -
Abstract: PMID: 2178839 -
Abstract: PMID: 2631673 Mathews TJ, Menacker F, MacDorman MF. Infant mortality statistics from the 2000 period linked birth/infant death data set. Nat Vital Stat Reports. 2002; 50(12): 12-13.5. -
Abstract: PMID: 20099209 Nylander PPS. (1978) Causes of high twinning frequencies in Nigeria. In: Navce WE, Allen G, Parisi P (eds) Twin Research: Biology and Epidemiology. Liss, New York, pp.35-43. -
Abstract: PMID: 6805197 -
Abstract: PMID: 2178836 -
Abstract: PMID: 10902821 -
Abstract: PMID: 5645958 Gersell DJ, Kraus FT. Disease of the placenta. In: Kurman RJ (ed) Blaustein’s pathology of the female genital tract. Springer-Verlag. New York, 1994 pp.975-1048. Pretorius DH, Mahony BS. Twin gestation. In: Nyberg DA, Mahoney BS, Pretorius DH (eds). Diagnostic Ultrasound of Fetal Anomalies. Mosby Year Book, St. Louis, 1990 pp.592-622. -
Abstract: PMID: 23208731 -
Abstract: PMID: 7506005 Gaziano EP, Harkness, UF. Doppler Velocimetry and Multiple Gestation. In: Doppler Ultrasound in Obstetrics and Gynecology. Maulik, D, ed. Springer-Verlag, Heidelberg, 2005. pp.313-320. -
Abstract: PMID: 21846456
6
8
13
14
17