Transvaginal Ultrasound: Information
Page Links: Introduction, Cervical Length, Preterm Labor, Preterm Labor Prediction, Progesterone Supplementation, Threatened Preterm Labor, Other Uses of Transvaginal Ultrasound, References
Introduction
This chapter is devoted to transvaginal ultrasound (TVUS) of the cervix. It includes a review of cervical length, preterm labor, preterm labor prediction, progesterone supplementation, threatened preterm labor, and other uses of transvaginal ultrasound.
Cervical Length
Transvaginal Cervical Length
Above. The transvaginal ultrasound measurement of cervical length leads to insights into the identification and treatment of a number of important clinical conditions, which range from preterm labor to induction of labor, prolonged pregnancies, timing of repeat C-sections, and management of polyhydramnios. The transvaginal ultrasound technique is superior to transabdominal and/or transperineal cervical length for usefulness and accuracy. [1]
Preterm Labor
Definition
The prevention of preterm labor (PTL) is one of the most important issues facing contemporary obstetrics.
Above. Defined as delivery occurring at less than 37 weeks, the worldwide incidence of preterm birth is 9.6%. [2]. Higher rates are reported for Africa and North America and lower rates for Europe. In addition, preterm delivery is responsible for higher rates of neonatal death and morbidity which extend into later life (bronchopulmonary dysplasia, brain injury) [3], and result in increased health care costs.
Above. About 30% to 35% of preterm births are related to medical indications, 40% to 45 % follow spontaneous premature labor, and 20% to 25% follow premature rupture of the membranes. Approximately 40% of preterm births occur at 33 weeks or less gestational age. [4]
Preterm Labor Causation
Spontaneous preterm birth is multifactorial and poorly understood. Regardless of etiology, its varying pathways lead to gross cervical changes commonly associated with early delivery, such as shortening, softening, and dilatation. [5] Solving the problem of preterm birth will require elucidation of molecular and biochemical events underlying the microstructural and biochemical changes that promote preterm birth. [6]
Strategies to Prevent Preterm Labor
Above. A number of strategies are proposed to prevent preterm birth. Preventive measures and interventions are possible. For example, efforts to reduce the frequency of multifetal pregnancies by reproductive health care practitioners and efforts to reduce induction of labor before 39 weeks are associated with reduced preterm births rates. Interventions such as progesterone supplementation and cervical cerclage also reduce the frequency of preterm birth. [7] Other strategies include tobacco control, fertility control, and dedicated prevention clinics. [8] Recently, the use of a vaginal pessary has been suggested as a means to reduce the risk of spontaneous preterm birth in certain populations.
Preterm Labor Prediction
Cervical Length and Preterm Labor (PTL) Prediction
Above. The detection of a short cervix by transvaginal ultrasound at 18 to 24 weeks gestation is the most powerful predictor of spontaneous preterm birth. [9] In a systematic review among asymptomatic women at increased risk for preterm birth, the most common transvaginal ultrasound cervical cutoff is < 25 mm to predict preterm birth at < 35 weeks gestation. [10] However, other critical cutoff values have been proposed to select women for certain therapeutic interventions.
Above. The cervical length during a normal pregnancy is > 30 mm.. A cervical length measured between 14 and 24 weeks gestation of 15 mm or less is associated with a 50% chance of preterm delivery at less than 33 weeks gestation. [11] In women with a prior spontaneous preterm birth, the shorter the cervix, the more likely recurrent preterm birth occurs. When the cervix is < 10 mm, there is a 90% chance of preterm birth before 35 weeks. [12]
Progesterone Supplementation
Above. Hassan and associates reported a 45% reduction in the rate of preterm singleton births before 33 weeks in women who received vaginal progesterone and who had a cervical length of 10 to 20 mm at 19 to 23 6/7 weeks. [13] A meta-analysis of 5 trials suggests that the administration of vaginal progesterone to women with a cervix of ≤ 25 mm is associated with a reduction in preterm birth at < 28 weeks, < 33 weeks, and < 35 weeks as well as fewer neonatal complications. [14] The natural vaginal progesterone daily dose among the studies was between 90 mg and 100 mg..
Routine Cervical Length Screening and Progesterone to Prevent Preterm Birth
The risk for preterm birth is decreased and perinatal outcomes are improved with the use of vaginal progesterone in singleton pregnancies with a mid-trimester cervical length of ≤ 25 mm and there is no evidence for adverse effects on neurodevelopment. [15]
The ACOG Practice Bulletin on Prediction and Prevention of Preterm Birth in 2012 (confirmed in 2014) recommends that progesterone supplementation should be offered to women at 16 to 24 weeks with a previous singleton preterm birth irrespective of cervical length, and in women who incidentally are noted to have a short cervix of ≤ 20 mm at or before 24 weeks. [16] While the Bulletin does not mandate universal screening, universal screening “may be considered.” This opinion is consistent with support for universal screening by others. [17] While the option to consider universal screening is open, Iams suggests that programs pursing this path must adhere to cost effectiveness, efficiency, and quality standards to ensure accurate measurements and treatment. [18] The Cervical Length Education and Review (CLEAR) entity is a credentialing program for cervical length measurement offered through the Perinatal Quality Foundation and can be found at: https://clear.perinatalquality.org/.
Finally, for twin and triplet pregnancies, a number of previous studies show no benefit for progesterone administration in the reduction of preterm labor. [19]
Summary: Critical Cervical Length for Treatment with Progesterone
If selective or universal screening is undertaken at 18 through 24 weeks and the transvaginal ultrasound cervical length is ≤ 20 mm, vaginal progesterone is initiated daily with 200 mg capsules or suppositories or 90 mg vaginal gel until 36 weeks. [20] Recent data suggests a cervical length cutoff of ≤ 25 mm..[21]
Cerclage and Progesterone
In a recent updated systematic review and adjusted indirect comparison meta-analysis, vaginal progesterone and cervical cerclage are equally effective for preterm birth prevention and for improvement in perinatal outcomes in women with a singleton gestation, spontaneous preterm birth and a mid-trimester sonographic short cervix. [22] Recent data also suggest that the outcomes of women who received both cervical cerclage and vaginal progesterone resulted in greater gestational age and birth weight compared to women who received cervical cerclage alone. [23]
Cervical length and Pessary
Among asymptomatic singleton pregnancies with a short cervix and no history of spontaneous preterm birth, the use of a pessary resulted in a lower rate of spontaneous preterm birth at <34 weeks. [24] Some data suggest that a cervical pessary may be similar in effectiveness to vaginal progesterone for the prevention of spontaneous preterm birth at less than 34 weeks in women with a short cervix. [25]
In a secondary analysis, of the Italian Pessary Trial asymptomatic singleton women with a short cervix performing moderate exercise (≥ 2 days per week) for ≥ 20 minutes had no increase in the risk for preterm delivery. [26] Women with a history of premature membrane rupture in a previous pregnancy, when treated with a pessary in the present pregnancy, may result in early delivery. [27]
Threatened Preterm Labor
Tsoi and colleagues found that the transvaginal cervical length (CL) at presentation in singleton women with intact membranes and threatened preterm labor (PTL)predicted delivery within 48 hours, within 7 days, and delivery at < 35 weeks. [28]
Above. When the CL was ≥ 15 mm no women delivered within 48 hours, and only 0.7% delivered within 7 days. These authors suggest that routine hospitalization may not be necessary in those with threatened preterm labor in the presence of a CL of ≥ 15 mm. Others also report a CL of ≥ 15 mm as the most relevant threshold for predicting delivery in women with threatened preterm labor. [29]
While CL is an independent predictor of preterm delivery in women with preterm labor, its predictive accuracy as a single measure is considered relatively limited by some. [30] In addition, the predictive accuracy for CL measurements among women with threatened PTL varies with gestational age at presentation with lower CL cutoff measurements noted at lower gestational ages. [31] Fetal fibronectin (fFn) testing may play a discriminating role in predicting PTL in these women.
Above. In women destined to deliver within 7 days, CL measurements, combined with fetal fibronectin testing improves identification of these women when the CL is between 15 and 30 mm. [32]
Above. The delivery risk between 7 and 14 days in women with threatened premature labor can be assessed by transvaginal CL and fFn performed on day 7 of women hospitalized for preterm birth. [33] The delivery risk between 7 and 14 days was increased in the presence of a CL of < 15 mm or a CL of ≥ 15 to 30 mm and a positive fFn compared with women with a CL of ≥ 30 mm..
Preterm Labor and the Risk for Preterm Delivery
Above. After preterm labor is arrested, women are at increased risk for preterm delivery if the cervix is ≥ 1 cm dilated by digital exam, < 15 mm CL on transvaginal ultrasound, and/or a positive fFn. [34]
Preterm Delivery Calculator
Above. The Center for Medical Statistics, Informatics, and Intelligent Systems (CeMSIIS) has created a statistical prediction model for individualized assessment for the risk of preterm delivery within 48 hours after transfer and before 32 weeks of gestation. [35] Data for the online calculator include: fetal fibronectin, transvaginal cervical length in mm, and C-reactive protein. A disclaimer is provided. This calculator can be accessed at the following link: CeMSIIS
See also QUiPP for preterm birth calculator information.
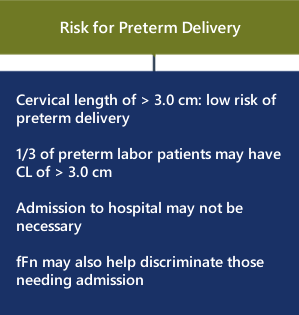
Low Risk for Preterm Delivery
Above. Women with a transvaginal cervical length of 3.0 cm or greater are unlikely to deliver prematurely despite admission for threatened premature labor. Over 1/3 of women with CL of > 3.0 cm are admitted unnecessarily to some hospital units with preterm labor. Yet, few or none deliver prematurely leading to inconvenience and cost. [36] The addition of fetal fibronectin testing in these women may be cost effective. [37]
Other Uses of Transvaginal Ultrasound
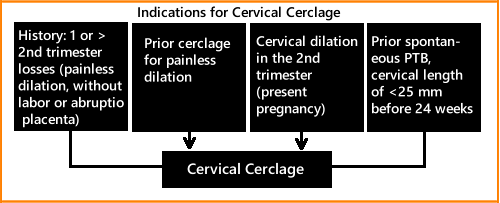
Cervical Cerclage and Preterm Delivery
Above. The ACOG Practice Bulletin on Cerclage for the Management of Cervical Insufficiency in 2014 suggests cerclage placement may be indicated in women with a singleton pregnancy who have a history of one or more second trimester pregnancy losses with painless dilatation and without labor or abruption placenta, history of prior cerclage for painless dilatation, and physical examination of cervical dilatation in the second trimester. [38] In addition, patients with prior spontaneous preterm birth, transvaginal cervical length of < 25 mm before 24 weeks may be candidates.
Cervical Length and Twins
Is second trimester cervical length (CL) a risk indicator for Cesarean delivery in twins? In this study, 311 women with a twin gestation attempted vaginal delivery after 34 weeks. Second trimester cervical length was measured in these women to determine if there were an association with the risk of emergency Cesarean section. In nulliparous women, there was no relationship between second trimester cervical length and Cesarean delivery. [39]
In a review of 5 randomized controlled trials, there is no evidence that cerclage is effective in multiple gestations in preventing preterm births, or in reducing perinatal deaths or neonatal morbidity. [40] However, a recent study suggests that in twin gestations, employing transvaginal ultrasound, the angle between the uterus and the cervix (uterocervical angle) of >110 degrees compared with the cervical length, may improve prediction for spontaneous preterm birth. [41]
Cervical Length and Induction of Labor
Above. The cervical length and Bishop score are significant predictors of successful induction of labor. Patients who deliver within 24 hours demonstrate a mean cervical length of 23.1 mm compared to women who deliver after 24 hours, who demonstrate a mean cervical length of 31.3 mm. [42] An independent predictor of C-section is a cervical length of 20 mm at the time of induction of labor at term. [43]
Transvaginal ultrasound of 1571 singleton low-risk pregnancies at 37 weeks predicted the onset and outcome of labor. [44] Women with a cervical length of 10 mm delivered at a mean gestation of 38 weeks, while those with a cervical length of 35 mm delivered at 41 weeks.
The following charts from the study’s abstract summarize the findings:

Above. Longer transvaginal cervical lengths measured at 37 weeks are associated with a higher incidence of delivery after 40 weeks and 10 days.
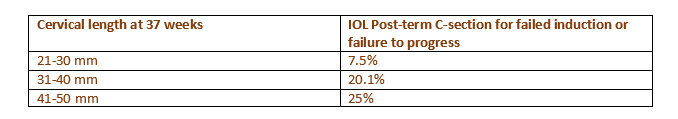
Above. Longer transvaginal cervical lengths measured at 37 weeks are associated with a higher rate of C-sections for failure to progress.
Cervical Length and Prolonged Pregnancy
Above. The chance for spontaneous labor at 41 weeks is greater in white, parous women and is greater when the maternal body mass index (BMI) is lower and when the sonographic cervix length is shorter. Further, these factors can define the probability of spontaneous labor and the risk of C-section in the week following the 41st week of pregnancy. [45]
In women undergoing induction of labor at 41 3/7 weeks to 42 1/7 weeks, a shorter sonographic cervical length and multiparity predicted the induction to delivery interval and the likelihood of vaginal delivery within 24 hours. [46]

Above. Transvaginal cervical length in women undergoing induction of labor at 41 3/7 to 42 1/7 weeks and the percent of those delivering within 24 hours according to parity. [47]
Cervical Length and Polyhydramnios
Other Considerations
- Intra-amniotic debris in asymptomatic nulliparous women with a transvaginal cervical length of <30 mm. have an increased risk for preterm birth before 34 and 32 weeks gestation. [48]
- Elastography is an imaging method which measures the characteristic of tissue to soften under pressure and may serve as an objective method to manage the risk for preterm labor. At present, no consensus has been achieved as to its” proper role. [49]
- Serial cervical length measurements in post-conization of the cervix in women without a short cervix may improve the prediction of spontaneous preterm birth. [50]
- Universal screening by vaginal ultrasound at 20 to 24 weeks is both feasible and acceptable to patients. [51] However, routine universal screening is presently not a part of all recommended guidelines.
Transvaginal Ultrasound: Imaging Considerations
Page Links: Measurement Technique Summary, Cervical Length Measurement, Sources of Error, Anatomic and Technical Pitfalls, References
Measurement Technique Summary
Above left. Note the appropriate anatomic landmarks for proper transvaginal ultrasound orientation.
Above right. Note the sequential steps for ultrasound performance. A review of image acquisition and technical performance for transvaginal ultrasound is also provided by these authors: [52]
Above left and right. Follow the imaging sequence as listed above.
Cervical Length Measurement
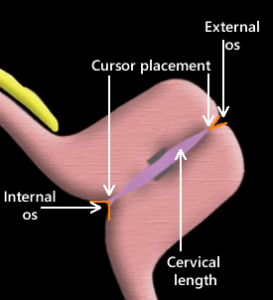
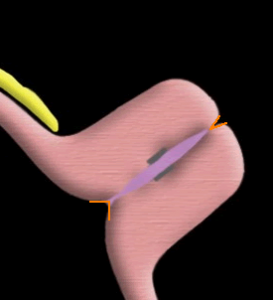
Above. When the mother is supine, the orientation of the vaginal ultrasound transducer probe in relationship to the position of the maternal feet and head is illustrated as well as the maternal orientation to posterior and anterior.
Above. Standard anatomic landmarks are the bladder, fetal presentation, cervical canal, internal cervical os, external cervical os, and vagina.
Above. Transvaginal ultrasound sagittal view of the cervix with the critical anatomic landmarks illustrated. The gain, zoom, and focal zone should be adjusted to optimize the image and a strict sagittal plane is necessary to image the entire cervix. The cervical canal is imaged horizontally in the middle of the screen, which may not be possible if the cervix is directly anterior.
Above. Once the cervical canal is identified, withdraw the probe slightly. Place the measurement cursors precisely at the closing points of the internal and external cervical os and measure the distance between them. For the internal os, a small triangle is often seen. Place the cursor at the apex of the triangle (the closing point). For the external os, follow the posterior cervical lip until the closing point is identified.
Sources of Error
1. Visualize the entire cervix
Above. The entire cervix is not visualized in this example and the internal cervical os and external cervical os is not well defined. Although the cervical length is probably normal, this is a suboptimal image.
2. Accurate cursor placement
Above. In the image above, the caliper placement is not exact and the distal cervix is not completely visualized, which hampers the recognition of the external cervical os.
3. Excessive probe pressure
Above. Avoid excess pressure on the probe and confirm that the thickness of the anterior and posterior lip of the cervix is the same. In the above example, there is dissimilarity between the thickness of the anterior and posterior cervical lips.
4. Lower uterine segment contractions
Above. Lower uterine segment contractions.
Above. Contractions may lead to an S-shaped canal and asymmetry of the anterior and posterior portions of the cervix.
5. Spontaneous cervical changes
Above. Progressive cervical shortening may occur after transabdominal pressure in patients at risk for cervical incompetence. [53]
Anatomic and Technical Pitfalls
In summary, a number of anatomic pitfalls are recognized and include: an underdeveloped lower uterine segment hampering the identification of the internal cervical os, focal myometrial contractions, spontaneous cervical change, and endocervical lesions such as polyps. [54] Technical pitfalls include incorrect interpretation due to vaginal probe orientation and due to cervical distortion by the probe.
Above. Transvaginal cervical length measurement training. A study shows that those with no prior training can adequately perform the transvaginal ultrasound exam after 18 consecutive ultrasound examinations, while those with experience required only 1 practice session to learn the technique. [55]
Transvaginal Ultrasound: Images
Above. This image represents a normal transvaginal cervical length with a proper sagittal view, distinct appearance of the distal cervix, and proper placement of the cursors for measurement.
Above. Cervical shortening on transvaginal ultrasound, and visualization of the amnion and chorion.
Above. Spontaneous change in apparent cervical length over a 2 minute observation interval.
Above. The membranes are filling the upper vagina. The approximate internal cervical os dilatation is 2.5 cm, and the approximate external cervical os dilatation is 5.2 cm.
Above. Breaking of the internal cervical os, and demonstration of the amnion and chorion.
Above. U-shaped funnel measuring 20 mm and cervical length measuring 21 mm.
Above. V-shaped funnel with short cervix. The distal cervix is poorly visualized in this image.
Above. An example of a transabdominal ultrasound of the cervical length in the presence of a distended maternal bladder. Compared to the transvaginal approach, this technique is not recommended to obtain accurate cervical length.
Above. Short cervix of 9.8 mm with cerclage sutures intact.
Above. This is a transabdominal cerclage image. The mersilene tape ligature is echogenic and there is no significant cervical shortening. Some ultrasound labs outline the endocervical canal, as illustrated, in the presence of a significantly curved canal, but preference should be given to measurement between cursors, except in extreme cases.
Transvaginal Ultrasound: Video
Above. The amniotic membranes remain intact, but are now filling the upper vagina.
Above. Extended V-shaped funnel resulting in a short cervix.
References
-
Abstract: PMID: 29220729 -
Abstract: PMID: 20428351 -
Abstract: PMID: 17762416 -
Abstract: PMID: 18177778 -
Abstract: PMID: 22717270 -
Abstract: PMID: 25084285 -
Abstract: PMID: 24806178 -
Abstract: PMID: 25477878 -
Abstract: PMID: 21879816 -
Abstract: PMID: 18412093 -
Abstract: PMID: 10871466 -
Abstract: PMID: 20708169 -
Abstract: PMID: 21472815 -
Abstract: PMID: 22284156 -
Abstract: PMID: 29157866 -
Abstract: PMID: 22996126 -
Abstract: PMID: 21472815 -
Abstract: PMID: 24807317 -
Abstract: PMID: 25731690 -
Abstract: PMID: 24807317 -
Abstract: PMID: 29157866 -
Abstract: PMID: 29630885 -
Abstract: PMID: 30140107 -
Abstract: PMID: 29260226 -
Abstract: PMID: 30204689 -
Abstract: PMID: 30173089 -
Abstract: PMID: 29920812 -
Abstract: PMID: 15736212 -
Abstract: PMID: 24342367 -
Abstract: PMID: 24201691 -
Abstract: PMID: 24907701 -
Abstract: PMID: 24807328 -
Abstract: PMID: 25845495 -
Abstract: PMID: 24839150 -
Abstract: PMID: 25616254 -
Abstract: PMID: 23816842 -
Abstract: PMID: 23791688 -
Abstract: PMID: 24451674 -
Abstract: PMID: 25402630 -
Abstract: PMID: 25208049 -
Abstract: PMID: 29190844 -
Abstract: PMID: 25123514 -
Abstract: PMID: 17444553 -
Abstract: PMID: 14689532 -
Abstract: PMID: 18816476 -
Abstract: PMID: 12858301 -
Abstract: PMID: 12858301 -
Abstract: PMID: 29155504 -
Abstract: PMID: -
Abstract: PMID: 30333498 -
Abstract: PMID: 29536576 -
Abstract: PMID: 17019742 -
Abstract: PMID: 9077619 -
Abstract: PMID: 10214824 -
Abstract: PMID: 17019742